New guidelines on Hospital Co-location by CMS
As the need for newer and more efficient care delivery models is rising, hospitals are moving towards the co-location concept where hospitals co-locate with other hospitals or healthcare entities. These space-sharing arrangements play a vital role in improving access to care in rural areas and help support visiting specialists in hospitals. But the lack of clear direction from CMS for co-location partnerships has been a concern among hospitals, with some hospitals even unwinding shared location or service arrangements. Earlier co-location guidance was limited to ad hoc interpretations by CMS or other state agencies, resulting in inconsistent interpretations and confusion regarding co-location permissibility.

In its final guidance, CMS has aimed to provide healthcare providers with information to help them make better decisions on partnering with other healthcare providers or entities in the co-location space. CMS has made some important revisions to allow and provide flexibility to hospitals and health systems to utilize co-location agreements. This will ultimately benefit patients and communities by improving the efficiency of healthcare services. CMS reiterated that each healthcare provider in the co-sharing space is responsible for ensuring safety and quality of care for patients and needs to demonstrate independent compliance with all Medicare and Medicaid program requirements.
In its final guidance, CMS has tried to remove some of the controversial aspects of the draft guidance like restrictions on co-usage of hospital space with space used by other healthcare entities, contracted nursing staff arrangements, and use of staff from a co-located hospital to provide rarely needed or emergency services. But improper guidance on critical access hospitals or private physician offices creates confusion.
CMS provides guidelines around regulatory requirements for hospitals to provide services in shared spaces. It asked the hospitals to remain vigilant and consider the risk of compliance through any shared space or service when partnering with other providers.
CMS outlined various acceptable arrangements, which are, a hospital may be co-located in its entirety, or only one part of a hospital such as its inpatient services or an outpatient department may be in another hospital’s building or on its campus. CMS also guided that an outpatient department may be co-located in an ambulatory surgical center, a rural health clinic, federally qualified healthcare center, imaging center, or other healthcare provider space.
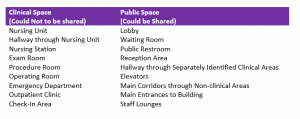
The guidance also provides specific instructions to surveyors to request and floor plans where floor plans must clearly distinguish the space used by the co-entities. CMS advised hospitals in co-location premises to carefully monitor instances of co-locations as an integral part of their survey readiness activities. CMS specified that Non-compliance found in the co-located surveyed space could be considered non-compliance for both entities.
CMS also brought guidance around contracted services such as laboratory, dietary, pharmacy, maintenance, housekeeping, and security and added that contracted services could include utilities such as fire detection and suppression and alarm systems. However, the document did not specify the services which cannot be contracted.
The guidance stated that the hospital is responsible for meeting staffing requirements by directly providing the staff or contracting staff from another entity. The guidance noted that contracted staff could only work for a single entity during any shift. In contrast, medical staff has been exempt from this limitation, provided that the medical staff holds privileges at both the entities in the co-location space. Also, when hospital staff is obtained from another provider, evidence that patients’ needs are being met is required.
While AHA has praised CMS for its flexible approach in co-location, health lawyers believe that the new guidelines create ambiguity around the requirements and lead to inconsistent results.
With the dynamic changing environment of the healthcare industry and new care delivery options coming up, you need an IT solution that provides a seamless experience for your healthcare staff and patients. Comes in, Elixir, the world’s first Practice Management solution built on the world’s #1 CRM and cloud solution, Salesforce. At Elixir, we understand the changing healthcare organizations’ needs, which is why we have developed a solution for you that provides seamless experience whether you are a multi-location, multi-service, or multi-care provider. Built on Salesforce’s open platform approach to API management, Elixir reduces interoperability stress on the system with coming regulatory changes.
Elixir Practice Management Suite is a comprehensive solution consisting of four modules that fit rightly into your healthcare business irrespective of your facility size and type. The Elixir Contact Center module helps manage the entire facility census and the patient intake process. At the same time, the Elixir EHR solution aims at delivering an end-to-end seamless patient care experience. The third module is Elixir Billing, and it effectively fetches data from any EHR platform to process medical claims and manages the entire revenue cycle. Elixir Patient Portal is the last module, and it provides an integrated experience for the patients.
Do fill out this contact form if you feel that Elixir will be an asset to enhancing your patient experience.
Recent Posts
Does Your Healthcare Solution Comply with HIPAA Regulations?
Integrated PDMP to help physicians address the opioid crisis
Categories
Recent Comments
Archives
- February 2025
- November 2024
- July 2024
- April 2024
- February 2024
- November 2023
- September 2023
- August 2023
- February 2023
- January 2023
- July 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- March 2021
- December 2020
- November 2020
- October 2020
- May 2020


